There were some extraordinary revelations at the Health Select Committee’s second evidence session of its (expanded) inquiry into the handling of NHS patient data on Tuesday 8th April.
This post is to draw attention to just one of them: a third opt-out form that the Health and Social Care Information Centre (HSCIC) has produced, on top of the two care.data opt-out codes you need to instruct your GP to add to your record.
The form that HSCIC has produced is dangerous. We don’t propose to link to it in case people download it, fill it in and accidentally de-register themselves from their GP!
In essence, HSCIC completely unnecessarily added a section to its form relating to a system called NHAIS (National Health Applications and Infrastructure Services) which if someone had completed – as many do when filling in complex forms, by signing wherever the form asks for a signature – would have meant they’d be de-registered by their GP and not be called for essential screening.
This exchange between Select Committee member Barbara Keeley MP and HSCIC Chair, Kingsley Manning gives you a sense of how this was viewed by the Committee:
Barbara Keeley MP: But it’s the way its phrased, it just looks like a threat. If you opt out…
Kingsley Manning: No, I agree, I agree…
Barbara Keeley MP: …your GP will drop you, and you’ll never have any screening.
Kingsley Manning: …I entirely agree.
You can download a safe version of the form, from which we have removed the offending section, via either of these links:
Withdrawal of Consent form (Microsoft Word format)
Withdrawal of Consent form (PDF format)
The Withdrawal of Consent form we provide should enable you to opt-out* of any one or more of the following ‘secondary use’ data sets, i.e. data sets that are not used for your direct medical care:
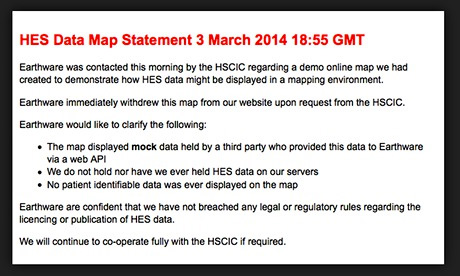
Hospital Episode Statistics (HES) – holds records on hospital episodes of care including inpatient, outpatient and A&E.
Secondary Uses Service (SUS) – the single source of comprehensive data for a range of reporting and analysis. NHS hospital trusts submit patient activity to SUS for performance monitoring, reconciliation and payments purposes.
Mental Health Minimum Data Set (MHMDS) – contains patient-level data about NHS services delivered to people with severe and enduring mental health problems.
Diagnostic Imaging Dataset (DIDS) – a central collection of detailed information about diagnostic imaging tests carried out on NHS patients, extracted from local radiology information systems.
*In this instance, ‘opt-out’ does not mean that your data will be deleted. Data held about you will instead be ‘anonymised’, i.e. items or links to anything that identifies you will be removed. For statistical audit purposes, NHS systems still require a de-identified record to exist.