…we’ve updated our scorecard.
One of the existing patient opt-outs has been renamed as the new National Data Opt-out, but a whole swathe of issues that have festered, unaddressed, for years still remain.
We consider these issues below, framed by questions of – and glaring omissions to – the ‘Your NHS Data Matters’ communications campaign, launched on GDPR Day.
Overview
“Your health and adult social care information supports your individual care. It also helps us to research, plan and improve health and care services in England.”
The word “us” appears to be doing a lot of work here; would patients expect “us” to include, for example, commercial information intermediaries such as Harvey Walsh Ltd?
“You can choose whether or not your confidential patient information is used for research and planning.”
All well and good, if true – but what about all other ongoing (and future) uses of patient information besides “research and planning”? Why does the new National Data Opt-out not use the far clearer, more accurate, and comprehensive Caldicott 3 definition of “purposes beyond direct care”?
If the new National Data Opt-out does cover the use of patients’ information for all purposes beyond their direct or ‘individual’ care, then why not say so? If it does not, then how does the ‘new’ opt-out meet the requirements of Caldicott 3, the recommendations of which the Government accepted in full?
medConfidential recommends: Be accurate! All public communications must in the first instance use the proper Caldicott 3 formulation, “purposes beyond direct care”.
These purposes may be further explained in terms of “research” and “planning”, but public explanations must be clear that uses are not limited to only these two purposes. To do otherwise would both mislead patients and undermine the effectiveness of the opt-out, and could lead to further collapses in public trust when people become aware of uses that do not clearly fall into either category.
“Information that only identifies you like your name and address is not confidential patient information and may still be used.”
This is utterly muddle-headed, and goes against what many (if not most) people reasonably understand is meant by the word “confidential”. While the example given is relatively benign it is precisely this loophole that, not coincidentally, led to the scandal of the Home Office MoU.
“Your confidential patient information is used in two different ways:”
This is not even close to true! We consider other uses, such as commissioning and commercial re-use in more detail below, but this statement is demonstrably untrue: take, for example, the HRA Confidentiality Advisory Group’s Non-Research Register, which contains ongoing uses such as invoice reconciliation, risk stratification, commissioning and projects that explicitly mix direct care and secondary uses.
medConfidential recommends: Don’t mislead patients! Be more clear and explicit about the range of uses to which patients’ information are put.
While public communications must be as clear and as understandable as possible, they must also be accurate – and true. The split between “your individual care” and “research and planning” (a description that we note above is itself too narrow and misleading) is far too simplistic, especially when patients are being asked to make an informed consent choice.
“Most of the time, we use anonymised data for research and planning. So your confidential patient information isn’t always needed.”
No definition of “anonymised” is provided. Using this word without explaining what it means is misleading; the natural (i.e. many patients’) assumption is that “anonymised data” is anonymous, which is not the case. GDPR and guidance from the ICO now makes it clear that what NHS Digital has been disseminating “most of the time” is identifiable data.
That only some identifiers are being removed, or pseudonyms substituted, must be explained – and linking to a third party, non-NHS information source to do this will hardly be reassuring to many patients. Hiding behind narrow legalistic reasoning and jargon never has and (especially post-GDPR) never will solve major long-standing issues.
medConfidential recommends: Follow the law! Stop implying that ‘anonymised’ is the same as anonymous, and respect people’s opt-outs for all identifiable data – don’t keep trying to find loopholes and excuses.
Benefits of data sharing
We are not aware that this is, or ever has been, in dispute. Clearly there are benefits to lawful, ethical, consensual, safe, and transparent data sharing.
Problems come when, as with the care.data programme and previous attempts at public communication, the NHS tries exclusively ‘selling the benefits’ without even mentioning any of the risks. Addressing these directly helps people make sense of the mitigations used – and such measures are no longer just arbitrary claims or assertions – and enables a more informed choice on that basis.
Who uses your data
As we note above, the narrow definition “research and planning” does not even come close to defining the full range of uses, for purposes beyond their direct care, to which patients’ information is put.
These omissions aside, and while ‘Your NHS Data Matters’ lists some types of organisations that may do “research” and acknowledges the use of patients’ information “to support the delivery of health and social care” (conflating both direct care and “planning”) it makes no mention of the types of organisations that may be involved in “planning”, and all of the activities that term is supposed to encompass.
Given that it is precisely those people and organisations that may have access to their information that matters to most patients who have concerns, this is another serious omission. Without it, how are patients supposed to make an informed choice?
medConfidential recommends: Be honest and upfront about who will have access to patients’ information; patients should not be assumed (or required) to understand the inner workings of the health and care system in order to make choices.
It may be argued that NHS Digital’s Data Release Register performs this function. However, linking to a massive Excel spreadsheet, containing literally thousands of individual entries, puts too much of a burden on any normal individual and – given the disparity between this and the level of detail provided elsewhere – begins to look like obfuscation.
We understand NHS Digital is working on a more clearly-formatted HTML publication of its Data Release Register but, in its absence, medConfidential has provided a more readable version that – unlike the current Register – contains links to NHS Digital’s audit reports, for those organisations that have been audited.
medConfidential recommends: Continue improving the transparency of data use.
For example, besides audits (and actions taken) future Registers should link to the relevant DARS and/or IGARD documentation; showing there is a process, and that the process is being applied competently and consistently is an important way to build and maintain trust.
It is unfortunate that the “NIC numbers” given in current Registers are entirely self-referential to anyone performing, e.g. a Google search; concealing or obscuring relevant parts of the process raises and persists doubts.
“Research bodies and organisations include:
– university researchers
– hospital researchers
– medical royal colleges
– pharmaceutical companies researching new treatments”
Why are “pharmaceutical companies” the only ones on this list whose use of patients’ information is qualified? Is the claim that pharmaceutical companies only receive patients’ data for the specific purpose of researching new treatments? This is patently untrue, and leads onto the further spurious claim that patients’ information will not be sold for “marketing or insurance” purposes.
While this claim may be narrowly true, at least for “commercial insurance purposes”, it omits to mention that at least some information intermediaries (i.e. commercial re-users, now sometimes referred to as “health and care analysis companies”) which regularly receive data from NHS Digital still service pharmaceutical marketers.
NHS Digital cannot state definitively who does or does not reuse patients’ medical records, as it specifically chooses not to know.
medConfidential recommends: Stop misleading patients as to the ultimate uses of their data, and stop sending out copies of everyone’s hospital histories to companies which (also) profit from servicing non-NHS commercial interests.
How data is protected
‘Your NHS Data Matters’ makes quite a few assertions about what will and will not be done with your data – though, and especially given the tendency to use jargon and narrow legalistic terms, it would be good to provide evidence and to clearly define key phrases. For example, we presume “confidential patient information” and “data” are two different things.
In addition, as noted above, linking to a third party, non-NHS information source to achieve some of this – however good the explanation – will hardly be reassuring to patients with concerns.
Another glaring omission, given the significant number organisations that do not provide health and care services, but that do use patients’ information for purposes beyond their direct care, is the list of the steps those organisations are supposed (required?) to take to protect patients’ data.
The list of steps for such organisations clearly cannot be the same as those for NHS bodies, in that some of these organisations do not “make it clear why and how data is being used”, and others hide behind the information intermediaries’ commercial reuse contracts to, e.g. measure the efficacy of pharma sales, and to market their products to NHS doctors and commissioners.
medConfidential recommends: Make it a requirement to report to NHS Digital (and thence to patients) how data is used by everyone; stop relying on commercial reuse contracts and the “promotion of health” loophole in the Care Act 2014 to persist what are self-evidently marketing uses.
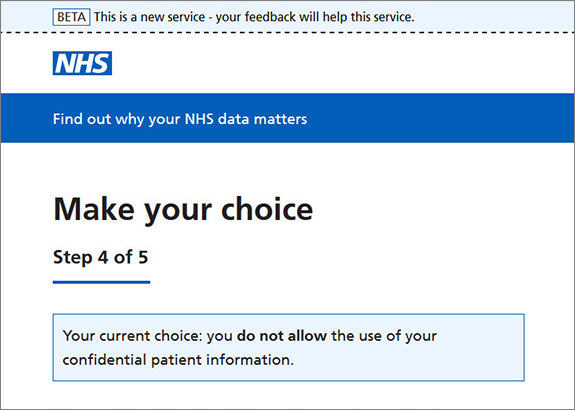
Manage your choice
The new ‘digital’ National Data Opt-out process cannot cope with dependant children, and assumes that all 13 year olds have mobile phones or e-mail accounts which can be accessed safely without duress. It appears as if, when the process was signed off under the Government’s Digital Service Standard, Ministers did not spare a thought for their families at all…
The entire process is overly bureaucratic and intimidating, especially when compared with the existing ‘Type-2’ opt-out process: rather than simply instructing your own GP, who already knows you, you must identify yourself to officials at a remote call centre – and may even have to send in up to four pieces of ID and documentation with a form. (Check pages 2-3 of NHS Digital’s 7-page ‘Non-Digital Proxy Opt-Out Form’ for a list of requirements.)
This feels more like an inquisition than a ‘choice’.
Given how fundamentally broken NHS Digital’s new ‘Beta’ opt-out process is, medConfidential recommends patients who have concerns use the opt-out form we’ve provided since late 2013.
We updated our form in line with recent changes and it still works for you, your dependant children and others for whom you are responsible – it also protects your GP data from uses beyond your direct care, not just your data supplied to NHS Digital.
With all that is and will be changing, medConfidential also strongly recommends you get yourself a Patient Online account, if you don’t already have one.
We provide more information about this on the ‘For patients’ section of our website.
Though it will still be some time until you can see how all of your data has been used, by which organisations and for what purposes, a Patient Online login to your GP’s online system should already allow you to see how your GP data is being used.
Where an opt out doesn’t apply
One critical question is whether patients’ opt-outs will now be honoured in the dissemination of ‘Hospital Episode Statistics’. HES comprises two-thirds of data releases from NHS Digital, most of those to commercial companies – including all of the commercial reusers. Until now, over 1.4 million patients’ wishes in this regard have been ignored.
Apparently officials believe IGARD, a body of NHS Digital’s own creation, can decide to override patients’ dissent when, in fact, the only body with a statutory basis to approve such exceptions is the Confidentiality Advisory Group (CAG) at the HRA.
Both GDPR and the UK’s new Data Protection Act clarify and extend the definition of identifiable data such that – the day before GDPR came into effect – staff at NHS Digital were ordered not to disseminate any “anonymised” patient data. Data releases were resumed the following day, but NHS Digital is still in discussions with the Information Commissioner’s Office as to what patient information can now be considered “anonymous”.
Under GDPR, this is unlikely to include HES in its current form: individual-level, lifelong hospital medical histories, where every event is dated and linked by a pseudonym.
Given a mother with two children is over 99% likely to be identifiable from her children’s birth dates alone, and given the enhanced GDPR ‘right of access’ to any data received by any customer of NHS Digital to which opt-outs have not been applied, it would seem not only unlawful but highly irresponsible for NHS Digital to keep selling what GDPR now defines as the identifiable patient data of those who have opted out.
If you – or any patient – would like to see how your data is used, and where your choices are being ignored, medConfidential recommends you visit TheySoldItAnyway.com